E. Cytoplasmic morphology assessment
E.1 Normal/granular
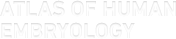
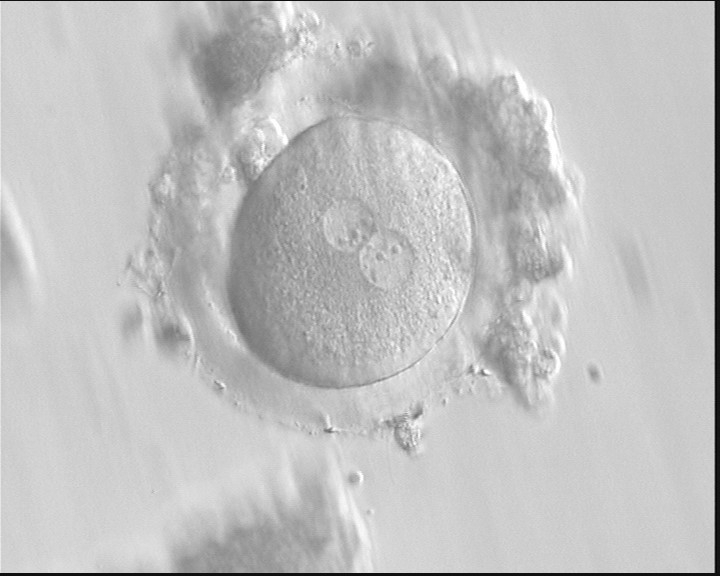
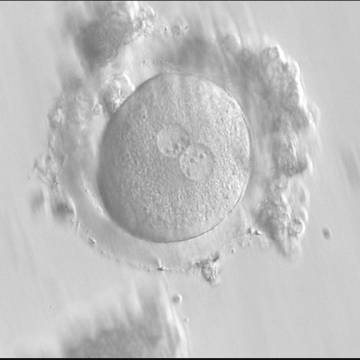
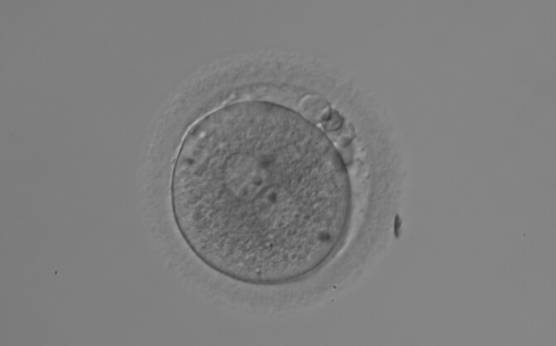
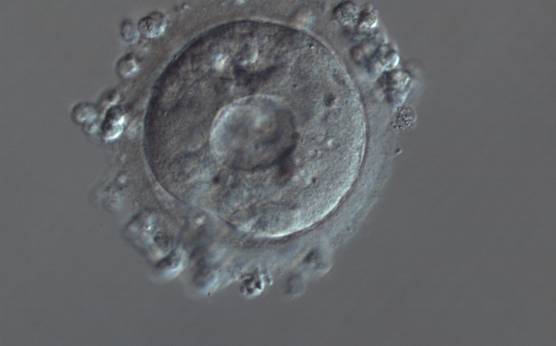
Homogeneous cytoplasm is expected in zygotes as for oocytes (Figs 190 and 191), but heterogeneous cytoplasm is of unknown developmental significance. Therefore, although some studies have reported that severe cytoplasmic anomalies in the zygote adversely affect the developmental and implantation potential of the resulting embryo (Kahraman et al., 2000; Ebner et al., 2003; Balaban and Urman, 2006), there is no clear evidence supporting these findings. Similarly, the presence of a peripheral cytoplasmic translucency in the fertilized oocyte (known as the ‘halo’; Fig. 192) or of minor dysmorphisms such as debris in the PVS (Fig. 193) or presence of refractile bodies in the cytoplasm (Fig. 194) have not been proved to be of prognostic value for implantation. Nevertheless, recording of these observations should be made as the accumulation of data could reveal some relevant links to developmental or implantation potential.
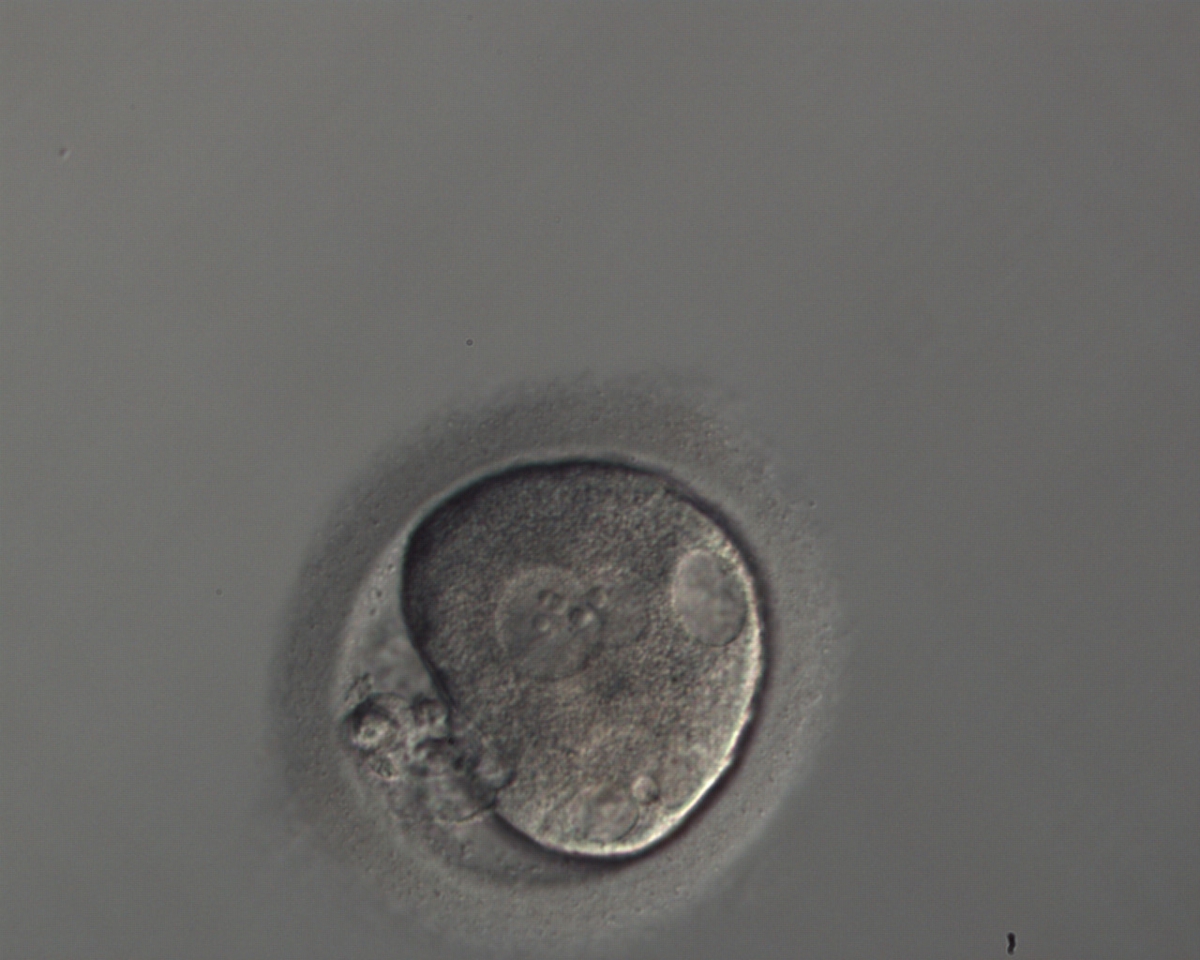
Normal cytoplasm is clearly distinguishable from granular cytoplasm, but to make comparative observations attention should be paid to the optical system and culture medium employed. The severity of granularity is generally based on the diameter and depth of the granular area that may occupy either the whole zygote (Fig. 195), or small (Figs 196–198) or large areas of the cytoplasm (Figs 199 and 200).
It has been reported that half of the oocytes with dysmorphic phenotypes such as organelle clustering are aneuploid, with hypohaploidy being the predominant abnormality (Van Blerkom and Henry, 1992). This severe cytoplasmic disorganization is associated with a lower intracytoplasmic pH and decreased ATP content (Van Blerkom et al., 1997). These dysmorphic changes would be inherited in the zygote. Apparently, intracytoplasmic organelle clustering (Fig. 200) is a type of severe abnormality that is significantly repetitive in consecutive cycles and is a negative predictor of pregnancy and implantation rates, although the cleavage stage embryo quality, as observed by light microscopy, is apparently not affected (Meriano et al., 2001).
E.2 Small vacuoles/large vacuoles
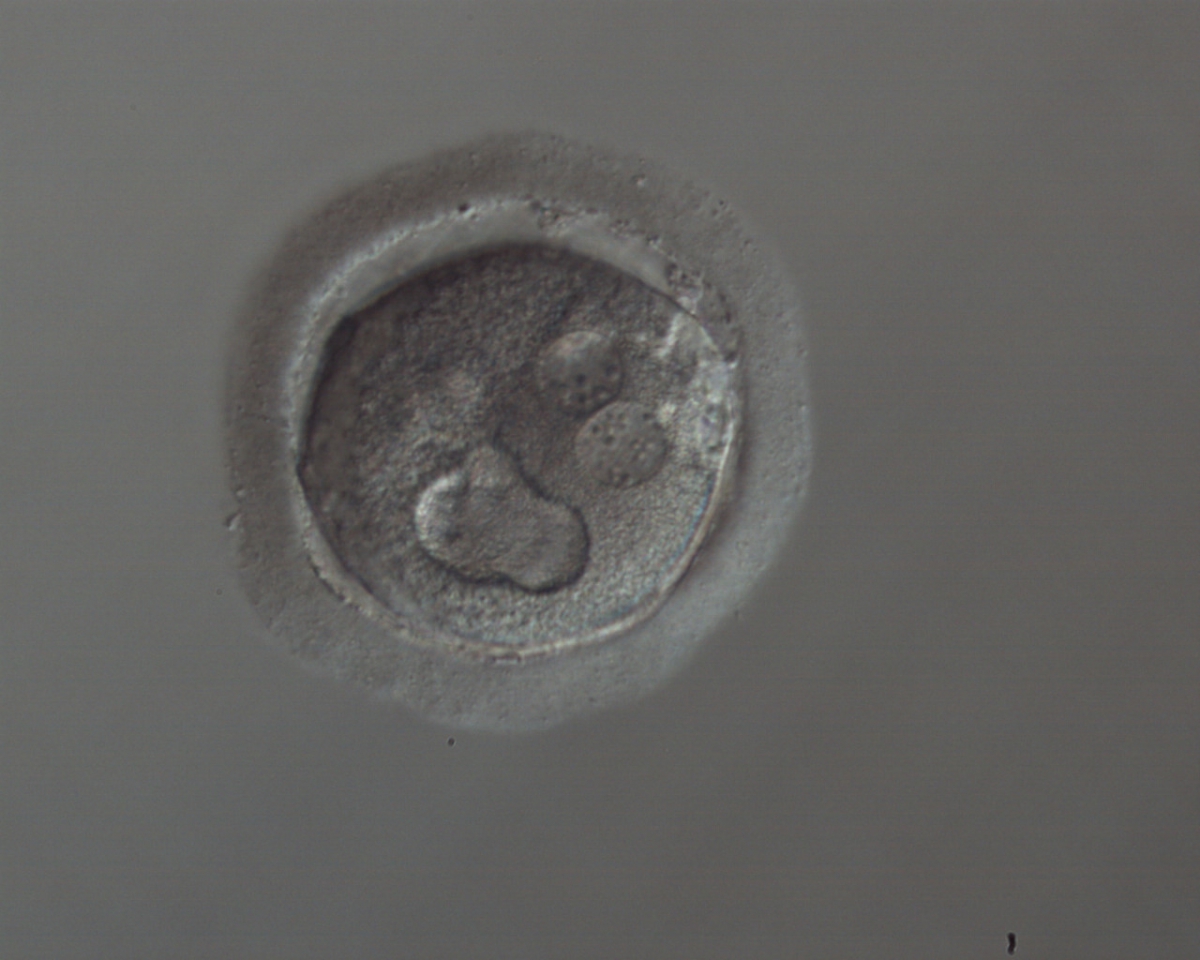
The presence of a few small vacuoles (diameter of 5–10 μm) that are apparently fluid filled and transparent (Figs 201 and 202) have not been associated with detectable biological consequences, but some concern may arise when several vacuoles appear (Figs 203 and 204) or appear with other morphological anomalies (Fig. 205).
Large vacuoles (>14 μm in diameter) in fertilized oocytes (Figs 206–210) can interfere with cleavage planes, resulting in reduced blastocyst formation (Ebner et al., 2005). For this reason, they are normally not considered for transfer.
At the time of fertilization check and especially after conventional IVF, it is extremely important to carefully score the cytoplasm for the presence of SER discs (see Chapter One), which are associated with the risk of a deleterious clinical outcome (Otsuki et al., 2004).
Article references:
Balaban B, Urman B. Effect of oocyte morphology on embryo development and implantation. Reprod BioMed Online 2006;12:608-615.
Medline | Web of Science | Google Scholar
Kahraman S, Yakin K, Dönmez E, Samli H, Bahçe M, Cengiz G, Sertyel S, Samli M, Imirzalioğlu N. Relationship between granular cytoplasm of oocytes and pregnancy outcome following intracytoplasmic sperm injection. Hum Reprod 2000;15:2390-2393.
Abstract/FREE Full Text
Ebner T, Moser M, Sommergruber M, Gaiswinkler U, Wiesinger R, Puchner M, Tews G. Presence, but not type or degree of extension, of a cytoplasmic halo has a significant influence on preimplantation development and implantation behaviour. Hum Reprod 2003;18:2406-2412.
Abstract/FREE Full Text
Ebner T, Moster M, Sommergruber M, Gaiswinkler U, Shebl O, Jesacher K, Tews G. Occurrence and developmental consequences of vacuoles throughout preimplantation development. Fertil Steril 2005;83:1635-1640.
CrossRef | Medline | Web of Science | Google Scholar
Meriano JS, Alexis J, Visram-Zaver S, Cruz M, Casper RF. Tracking of oocyte dysmorphisms for ICSI patients may prove relevant to the outcome in subsequent patient cycles. Hum Reprod 2001;16:2118-2123.
Abstract/FREE Full Text
Otsuki J, Okada A, Morimoto K, Nagai Y, Kubo H. The relationship between pregnancy outcome and smooth endoplasmic reticulum clusters in MII human oocytes. Hum Reprod 2004;19:1591-1597.
Abstract/FREE Full Text
Van Blerkom J, Henry G. Oocyte dysmorphism and aneuploidy in meiotically mature human oocytes after ovarian stimulation. Hum Reprod 1992;7:379-390.
Abstract/FREE Full Text
Van Blerkom J, Antczak M, Schrader R. The developmental potential of the human oocyte is related to the dissolved oxygen content of follicular fluid: association with vascular endothelial growth factor levels and perifollicular blood flow characteristics. Hum Reprod 1997;12:1047-1055.
Abstract/FREE Full Text